Cystoscopy
What is a Cystoscopy?
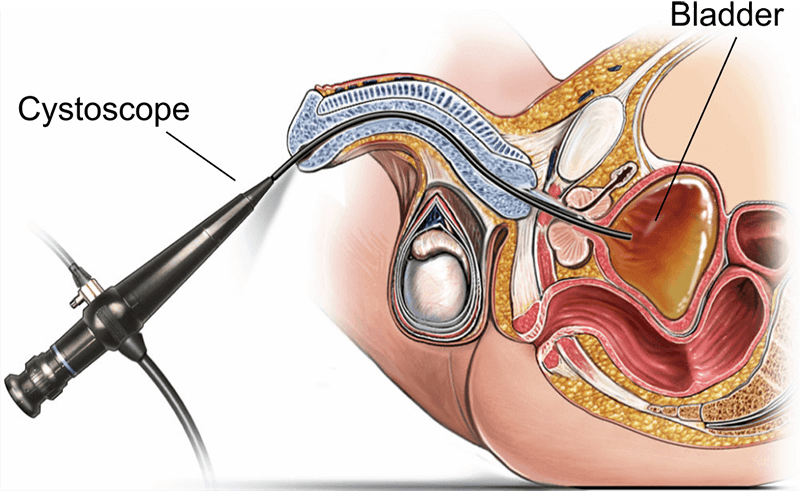
Cystoscopy is a diagnostic procedure used to assess the extent of prostate enlargement and the complete lower urinary tract. During a cystoscopy, a thin, flexible tube with a camera at the end, called a cystoscope, is inserted into the urethra and advanced into the bladder. This allows the doctor to visualise the bladder wall and urethra, identify abnormalities, and sometimes perform treatments.
Who is Suitable for a Cystoscopy?
While cystoscopy is not routinely performed for all patients with BPH, it may be recommended for the following individuals:
- Suppose you are experiencing severe urinary symptoms associated with BPH, such as urinary retention (inability to urinate), recurrent urinary tract infections, or haematuria (blood in the urine). In that case, your doctor may suggest a cystoscopy to evaluate the underlying cause.
- Suppose conservative measures such as lifestyle changes, medications, or minimally invasive procedures have failed to adequately relieve your symptoms. In that case, cystoscopy may be warranted to assess the need for more invasive treatments, such as surgery.
- Suppose surgical intervention is being considered for the management of BPH. In that case, cystoscopy may be performed to assess the size and configuration of the prostate gland and the condition of the bladder and urethra. This information helps the urologist plan the most appropriate surgical approach.
- Recurrent urinary tract infections or complications such as bladder stones or diverticular may indicate underlying bladder dysfunction secondary to BPH. Cystoscopy can help identify these issues and guide treatment decisions.
- In some cases, other conditions, such as bladder cancer or urethral stricture, can present with symptoms similar to BPH. Cystoscopy allows for direct visualisation of the urinary tract, helping to confirm the diagnosis and rule out other possible causes of symptoms.

Benefits of Cystoscopy
- Accurate Assessment: Cystoscopy provides direct visualisation of the prostate gland, allowing for an accurate assessment of its size, shape, and any associated abnormalities. This information is crucial for determining the severity of BPH and guiding treatment decisions.
- Identification of Complications: Cystoscopy helps identify complications associated with BPH, such as bladder diverticulae, bladder stones, or urethral strictures. Early detection of these complications allows for timely intervention and prevention of further complications.
- Guidance for Treatment Planning: Cystoscopy visualises the prostate gland and assesses bladder function, helping urologists determine the most appropriate treatment approach for BPH. This may include medication, minimally invasive procedures, or surgical intervention.
- Confirmation of Diagnosis: In cases where the diagnosis of BPH is uncertain or other conditions are suspected, cystoscopy can help confirm the diagnosis by visualising the prostate gland and ruling out other possible causes of urinary symptoms.
- Monitoring of Disease Progression: For individuals with BPH who require ongoing management, cystoscopy can be used to monitor disease progression and assess the effectiveness of treatment over time. This allows for adjustments to treatment plans as needed to optimise outcomes.
- Patient Education: Cystoscopy allows patients to see the condition of their prostate gland visually and understand the underlying causes of their urinary symptoms. This can empower patients to take an active role in their treatment decisions and management of BPH.
Types of Cystoscopy
- Flexible Cystoscopy: is the most common type of cystoscopy used to evaluate BPH. A thin, flexible cystoscope is inserted through the urethra and advanced into the bladder. This type of cystoscopy is well-tolerated by most patients and can be performed in an outpatient setting with minimal discomfort.
- Rigid Cystoscopy: In some cases, a rigid cystoscope may be used for cystoscopy, especially if additional instrumentation or treatment is needed. Rigid cystoscopy uses a straight, rigid instrument to visualise the bladder and urethra. While it may be slightly more uncomfortable than flexible cystoscopy, it allows for better visualisation and manipulation of instruments within the urinary tract.
Preparation Before a Cystoscopy
- Discuss Medications: Talk to your doctor about any medications you're taking, including prescription drugs, over-the-counter medications, and supplements. Some medicines may need to be adjusted or temporarily stopped before the procedure.
- Provide Medical History: Your doctor will likely ask about your medical history, including previous surgeries, allergies, and current health conditions. Be sure to provide accurate information to help ensure your safety during the procedure.
- Arrange Transportation: Since you may receive sedation or anaesthesia for the procedure, it's important to arrange for someone to drive you home afterwards. Due to the effects of the sedation, you may not be able to drive yourself.
- Follow Fasting Instructions: Depending on the type of anaesthesia used, you may be instructed to avoid eating or drinking for a certain period before the procedure. Follow your doctor's instructions closely to minimise the risk of complications.
- Plan for Recovery: Arrange for someone to assist you at home after the procedure, especially if you anticipate needing help with daily activities or transportation.
Cystoscopy Procedure
- Preparation: You'll be asked to change into a hospital gown and empty your bladder before the procedure begins.
- Anaesthesia: Depending on the type of cystoscopy and your needs, you may receive local anaesthesia to numb the area or general anaesthesia to put you to sleep during the procedure. Your doctor will discuss the options with you beforehand.
- Insertion of Cystoscope: The urologist will gently insert a cystoscope, a thin, flexible tube with a camera at the end, into your urethra and advance it into your bladder. This may cause discomfort or pressure, but it shouldn't be painful, especially if anaesthesia is used.
- Visualisation: As the cystoscope advances, the urologist will visually inspect the bladder and prostate gland to assess their size, shape, and abnormalities. They may also examine the urethra for signs of obstruction or other issues.
- Assessment and Treatment: If abnormalities are detected during the cystoscopy, the urologist may perform additional tests or procedures, such as taking tissue samples (biopsies), removing bladder stones, or treating urinary symptoms.
What to Expect After a Cystoscopy?
- Recovery: After the procedure, you'll be taken to a recovery area where you can rest until the effects of the anaesthesia wear off. You may experience some mild discomfort or urinary symptoms, such as burning with urination or the need to urinate more frequently. These symptoms typically improve within a day.
- Follow-up Instructions: Your doctor will provide specific instructions for your recovery, including any medications to take, activity restrictions, and signs of potential complications to watch for. Follow these instructions closely to ensure a smooth recovery.
- Results: If tissue samples were taken during the cystoscopy, receiving them may take a few days. Your doctor will discuss the findings with you and recommend any necessary follow-up or treatment.
- Resumption of Activities: Most people can resume their normal activities within a day or two after a cystoscopy, although you may need to avoid strenuous exercise or heavy lifting for a short time.
- Follow-up Appointment: Depending on the cystoscopy results and your individual needs, your doctor may schedule a follow-up appointment to discuss further treatment options or monitor your condition over time.
Cystoscopy Risks
While cystoscopy is generally considered a safe procedure, there are some risks and potential complications to be aware of, including:
- Urinary Tract Infection (UTI): There is a risk of developing a UTI following cystoscopy, especially if the bladder is filled with a sterile solution during the procedure.
- Bleeding: It's not uncommon to experience some minor bleeding after cystoscopy, particularly if tissue samples (biopsies) are taken or if treatments such as bladder stone removal are performed.
- Injury to the Urethra or Bladder: In rare cases, cystoscopy may cause injury to the urethra or bladder, leading to bleeding, infection, or other complications.
- Urinary Retention: Some individuals may experience difficulty emptying their bladder following cystoscopy, leading to temporary urinary retention.
- Allergic Reaction: Although rare, there is a slight risk of allergic reactions to medications or materials used during the procedure.
What if Cystoscopy is Delayed?
If cystoscopy for an enlarged prostate is delayed, it may result in delayed diagnosis and treatment of BPH or any associated complications. While a short delay may not significantly impact prognosis, prolonged delay can lead to worsening urinary symptoms, decreased quality of life, and an increased risk of complications such as urinary retention, bladder stones, or recurrent urinary tract infections.
If you're experiencing symptoms suggestive of BPH or have concerns about your prostate health, it's important to discuss them with your urologist promptly.







