What is AN Enlarged Prostate?
About Benign Prostatic Hyperplasia (BPH)
Enlarged prostate, also known as benign prostatic hyperplasia (BPH), is a common condition among ageing men. It occurs when the prostate gland, which surrounds the urethra and is located just below the bladder, enlarges.
As men age, the prostate gland tends to enlarge. This growth is generally benign but can lead to compression of the urethra, causing urinary symptoms.
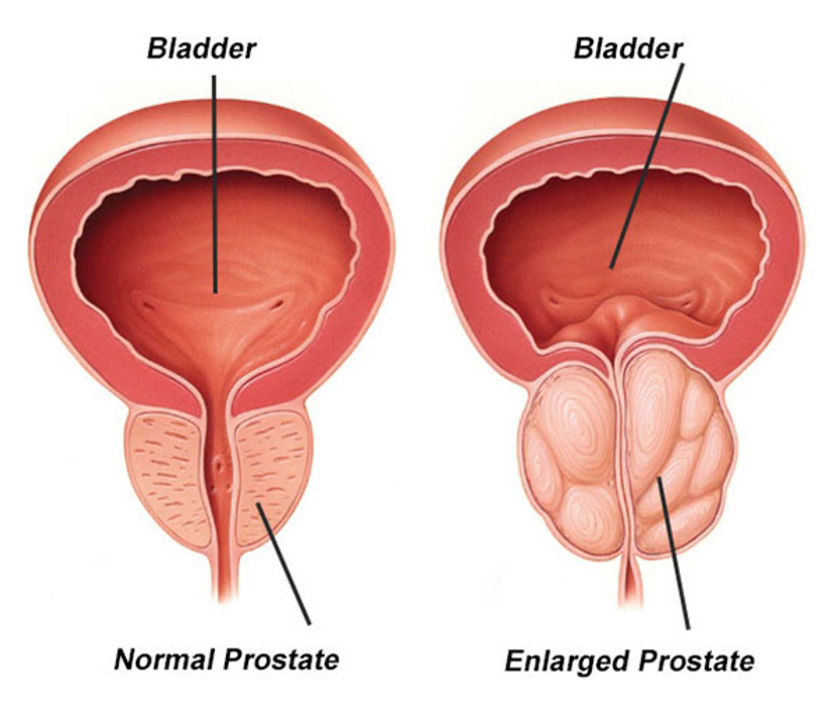
Impact of BPH on Anatomy and Health
- Urinary Symptoms: An enlarged prostate can lead to urinary symptoms due to the pressure it puts on the urethra. These symptoms may include increased frequency of urination, difficulty starting urination, weak urine stream, dribbling at the end of urination, and incomplete bladder emptying.
- Urinary Tract Infections (UTIs): In some cases, incomplete bladder emptying can increase the risk of urinary tract infections.
- Bladder Stones: The increased risk of urinary retention can lead to the formation of bladder stones.
- Bladder Damage: Chronic urinary retention can cause the bladder muscle to stretch and weaken over time, leading to bladder damage.
- Acute Urinary Retention: In severe cases, BPH can lead to acute urinary retention, where the individual is unable to urinate at all. This requires immediate medical attention and may necessitate the insertion of a catheter to drain the bladder.
- Quality of Life Impact: The urinary symptoms associated with an enlarged prostate can significantly impact a man's quality of life, leading to frustration, embarrassment, and limitations on daily activities.
Causes and Risk Factors for Benign Prostatic Hyperplasia
- Age: BPH is primarily a condition of ageing. As men get older, the prostate gland tends to enlarge gradually. It's estimated that by age 60, over half of men will have some degree of prostate enlargement, and by age 85, this percentage increases to about 90%.
- Family History: Men with a family history of BPH are more likely to develop the condition themselves.
- Hormonal Changes: Changes in hormonal balance, particularly the increase in dihydrotestosterone (DHT) levels with age, may contribute to prostate growth.
- Medical Conditions: Certain medical conditions, such as obesity and diabetes, have been associated with an increased risk of BPH.
- Lifestyle Factors: Certain lifestyle factors, including obesity, lack of physical activity, and poor diet, may also influence the development of BPH.
Symptoms of Benign Prostatic Hyperplasia
The symptoms of enlarged prostate can vary in severity and may include:
- Urinary Symptoms:
- Increased frequency of urination, especially at night (nocturia)
- Difficulty starting urination (hesitancy)
- Weak urine stream
- Dribbling at the end of urination
- Sensation of incomplete bladder emptying
- Straining to urinate
- Urinary urgency
- Urinary Tract Infections (UTIs): In some cases, incomplete bladder emptying due to BPH can increase the risk of urinary tract infections.
- Bladder Stones: Chronic urinary retention associated with BPH can lead to the formation of bladder stones.
- Bladder Damage: Over time, chronic urinary retention can stretch and weaken the bladder muscle, causing bladder damage.
- Acute Urinary Retention: In severe cases, BPH can lead to acute urinary retention, where the individual is unable to urinate at all. This is a medical emergency and requires immediate attention.
Diagnosis of Benign Prostatic Hyperplasia
Here are the common steps involved in diagnosing BPH:
- Medical History and Physical Examination: The doctor will ask about the individual's medical history, including urinary symptoms and other relevant medical conditions. A digital rectal examination (DRE) may be performed to assess the prostate gland's size, shape, and consistency.
- Symptom Assessment: The International Prostate Symptom Score (IPSS) questionnaire may be used to assess the severity of urinary symptoms and their impact on quality of life.
- Diagnostic Tests:
- Prostate-Specific Antigen (PSA) Test: A blood test may be done to measure PSA levels. While elevated PSA levels can indicate prostate conditions such as BPH or prostate cancer, BPH itself does not cause an elevation in PSA levels.
- Urinalysis: A urine sample may be analysed for signs of infection or other urinary abnormalities.
- Uroflowmetry: This test measures the rate and volume of urine flow, providing information about urinary function and possible obstruction.
- Ultrasound: This imaging test uses sound waves to create a picture of the prostate gland, allowing healthcare providers to assess its size and detect abnormalities.
- Cystoscopy: In some cases, a thin, flexible tube with a camera (cystoscope) may be inserted into the urethra to visualise the prostate and bladder.
- Rule Out Other Conditions: Since the symptoms of BPH can mimic those of other urinary conditions, such as urinary tract infections or prostate cancer, additional tests may be done to rule out these conditions.
Treatment Options for Benign Prostatic Hyperplasia
- Monitoring: An observational approach may be appropriate for men with mild symptoms or those not significantly bothered by their symptoms. Regular monitoring of symptoms and prostate size may be recommended, and treatment may be initiated if symptoms worsen over time.
- Lifestyle Changes: Making certain lifestyle modifications can help alleviate symptoms of BPH and improve urinary function. These may include:
- Limiting fluid intake before bedtime to reduce nighttime urination (nocturia).
- Avoiding caffeine and alcohol, which can irritate the bladder and worsen urinary symptoms.
- Maintaining a healthy weight through diet and exercise, as obesity can exacerbate BPH symptoms.
- Practising pelvic floor exercises, such as Kegel exercises, to improve bladder control.
- Medications: Several classes of medications may be prescribed to manage symptoms of BPH, including:
- Alpha-blockers: These medications relax the prostate and bladder neck muscles, improve urine flow, and reduce symptoms such as urinary hesitancy and weak stream.
- 5-alpha reductase inhibitors: These medications reduce the production of dihydrotestosterone (DHT), which can help shrink the prostate gland over time and improve urinary symptoms.
- Combination therapy: Some individuals may benefit from a combination of alpha-blockers and 5-alpha reductase inhibitors for more comprehensive symptom relief.
- Other medications: Additional medications, such as anticholinergics or phosphodiesterase-5 inhibitors, may be prescribed to address specific symptoms or complications associated with BPH.
- Minimally Invasive Procedures: Minimally invasive procedures may be considered for individuals who do not respond adequately to medications or who prefer to avoid surgery. These procedures aim to reduce prostate tissue and relieve urinary obstruction without the need for major surgery. Examples of minimally invasive procedures for BPH include Rezum steam therapy and prostatic urethral lift (UroLift).
- Surgery: In severe symptoms or complications such as urinary retention, surgical intervention may be necessary to relieve urinary obstruction and improve urinary flow. Laser prostate surgery (HoLEP) or transurethral resection of the prostate (TURP) is the most common surgical procedure for BPH. It involves removing excess prostate tissue through a scope inserted into the urethra.
What if Benign Prostatic Hyperplasia is Untreated?
If left untreated, BPH can lead to worsening urinary symptoms and complications that can significantly impact quality of life and overall health. Some potential consequences of untreated BPH include:
- Acute Urinary Retention (AUR)
- Chronic Urinary Retention
- Kidney Damage
- Decreased Quality of Life
- Increased Risk of Complications
Early diagnosis and appropriate management of BPH are essential for minimising symptoms, reducing the risk of complications, and improving quality of life. Regular follow-up with a urologist is important for monitoring the condition and adjusting treatment as needed.








